Motion Preservation of the Spine – Disc Replacement
Spinal health plays a crucial role in maintaining overall mobility, function, and quality of life. When spinal degeneration or injury occurs, patients often face chronic pain and limited movement.
Traditional treatments, such as spinal fusion, have been effective in reducing pain but often come at the cost of decreased spinal motion. In contrast, motion-preserving procedures like total disc replacement (TDR) offer an alternative that aims to maintain the natural biomechanics of the spine while alleviating pain. In this newsletter, we’ll explore the concept of motion preservation in spinal care, delve into the history and evolution of disc replacement technology, examine its benefits and risks, and discuss the future of this innovative approach to spinal surgery.
The Concept of Motion Preservation in Spinal Surgery
Motion preservation in spinal surgery refers to techniques that restore function while maintaining the natural movement of the spine. Unlike spinal fusion, which permanently joins vertebrae to stabilize the spine, motion-preserving procedures aim to preserve flexibility, reduce adjacent segment disease (ASD), and improve patient outcomes.
Why Motion Preservation Matters
The spine is a highly dynamic structure composed of vertebrae, intervertebral discs, ligaments, and muscles that work together to support movement and absorb impact. When one segment of the spine becomes immobilized through fusion, it alters the mechanics of surrounding segments, potentially accelerating wear and tear on adjacent discs and leading to additional degenerative changes. Motion-preserving techniques, such as total disc replacement, attempt to minimize these issues by maintaining near-normal movement patterns.
Understanding Disc Replacement Surgery
What is Total Disc Replacement (TDR)?
Total disc replacement (TDR), also called artificial disc replacement, is a surgical procedure that involves removing a damaged intervertebral disc and replacing it with an artificial one. The goal is to relieve pain while allowing continued motion at the treated spinal segment. TDR is commonly performed in the cervical (neck) and lumbar (lower back) regions, as these are the most mobile and commonly affected spinal areas.
How Does Disc Replacement Work?
1. Surgical Approach – The procedure is typically performed through an anterior approach (from the front) to minimize disruption to spinal muscles and posterior structures.
2. Disc Removal – The surgeon carefully removes the degenerated or damaged disc while preserving as much of the surrounding structures as possible.
3. Implant Placement – The artificial disc, designed to mimic the function of a natural disc, is inserted into the space between the vertebrae.
4. Post-Surgical Integration – Over time, the artificial disc integrates with the surrounding vertebrae, restoring motion while maintaining spinal alignment.
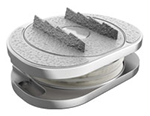
Types of Artificial Discs
Artificial discs come in various designs, but they generally fall into two main categories: • Metal-on-Polymer – Comprising a metal endplate and a polyethylene (plastic) core, these designs mimic the function of natural discs by allowing controlled motion. • Metal-on-Metal – Featuring metal components that articulate with each other, these designs provide durability and stability. Different devices are used for the cervical and lumbar spine, with the choice depending on factors such as anatomy, severity of degeneration, and surgeon preference.
History and Evolution of Disc Replacement
Early Research and Development The concept of artificial disc replacement has been around since the 1960s, but it wasn’t until the 1980s and early 1990s that significant advancements in biomaterials and surgical techniques made it a viable alternative to spinal fusion. The first widely used artificial disc, the SB Charité, was developed in Germany and received approval in the early 2000s. Since then, numerous designs have been introduced, improving longevity, biomechanics, and patient outcomes. FDA Approval and Adoption • 2004: The FDA approved the Charité artificial disc for lumbar disc replacement, marking a milestone in spinal surgery. • 2007: The ProDisc-L received FDA approval, providing another lumbar option. • 2013-Present: Cervical disc replacements such as M6 Disc Replacement, Mobi-C and Prestige LP gained traction, leading to an increase in cervical disc arthroplasty procedures. Today, disc replacement has become a well-established procedure, particularly for patients with degenerative disc disease who wish to maintain motion while alleviating pain.
Benefits of Disc Replacement Surgery
Motion Preservation
Unlike spinal fusion, which eliminates movement at the treated segment, disc replacement maintains near-normal spinal motion, reducing strain on adjacent levels.
Reduced Adjacent Segment Disease (ASD)
Fusion increases stress on the discs above and below the treated level, often leading to further degeneration. Studies suggest that TDR significantly reduces the risk of ASD compared to fusion.
Faster Recovery and Rehabilitation
Patients undergoing disc replacement often experience a quicker return to function, as the procedure minimizes disruption to spinal structures. Many resume daily activities within weeks.
Long-Term Durability
Modern artificial discs are designed to withstand years of use, with clinical studies showing durability over a decade in many cases.
Improved Patient Satisfaction and Outcomes
Many people are more happy with TDR than with fusion. This is most of all true for less pain and how they can move.
Who Can Get a Disc Replacement?
Disc replacement works best for people who:
✅ Have single-level degenerative disc disease with a firm back
✅ Have long-term back or neck pain that did not get better with other care
✅ Have good bones and a straight spine
✅ Are less than 60 years old (but old people can still be a fit if they are well)
But, people with very bad joint pain, a past back fix, or a back that is not the right shape may not be a good fit for TDR.
Disc Replacement vs. Spinal Fusion: A Look at Both
Both ways to fix the back can work well. But disc replacement is often the first choice when it is key to keep the back able to move.
The Future of Motion Preservation and Disc Replacement
Newer Biomaterials
New parts are made from things that are safe for the body. This will help them last a long time and work very well.
More Uses for It
With new study, disc replacement may be a good choice for more than one bad disc. It may also be good for old people. This will make it a more used way to care for the spine.
Motion preservation in back care is a big change in how we fix degenerative disc disease and long-term back pain. Total disc replacement is a very good choice other than spinal fusion. It lets you move and takes away pain. As we find new ways to do things, the new disc will get even better. It will give people a safe fix that lasts a long time for their back.
If your back or neck hurts all the time, you have choices. Talk to a back doctor. They can tell you if a disc replacement is a good choice for you. Know the facts. Keep on the move. And be in charge of your back's health